
Consent for Blood Transfusion is a crucial process where patients are informed about the risks, benefits, and alternatives before receiving blood products. This ensures that patients voluntarily agree to the procedure, understanding potential complications such as allergic reactions or infections. Proper documentation of consent for blood transfusion protects both the patient's rights and the healthcare provider's legal responsibilities.
Informed Consent for Blood Transfusion
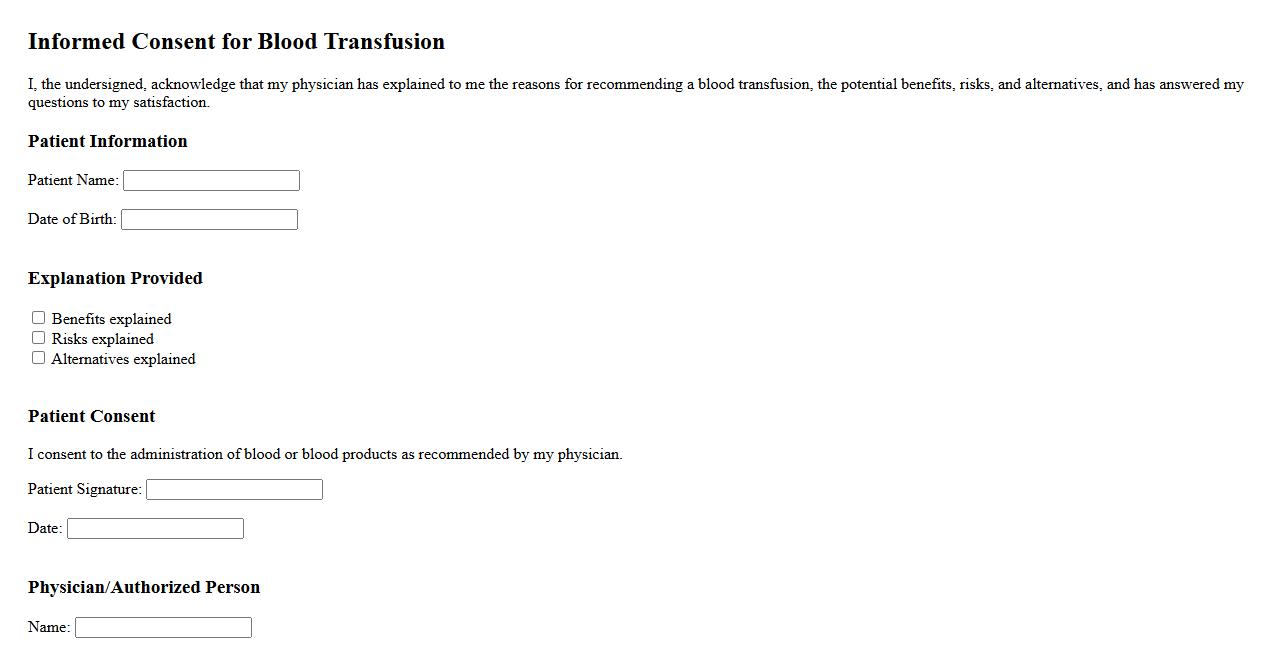
Informed consent for blood transfusion is a critical process where patients receive comprehensive information about the procedure, risks, and benefits before agreeing to treatment. This ensures that individuals make educated decisions regarding their healthcare. Proper documentation of consent protects both the patient's rights and healthcare providers' responsibilities.
Parental/Guardian Consent for Blood Transfusion
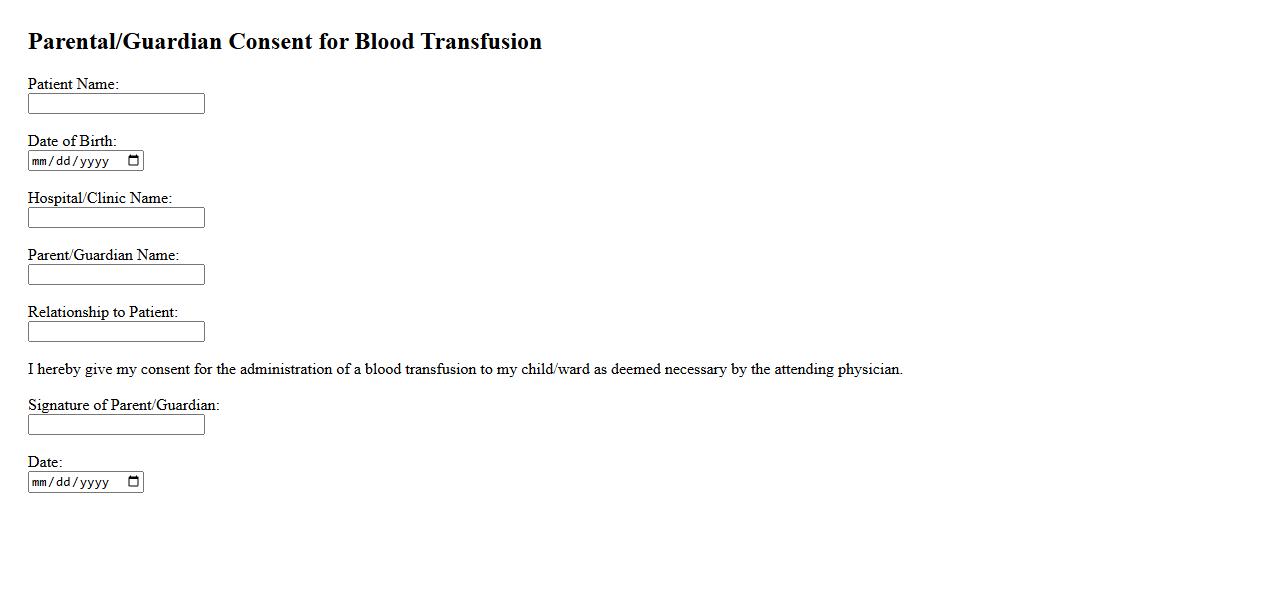
Parental/Guardian Consent for Blood Transfusion is a crucial legal document that ensures the approval of a parent or guardian before a minor receives a blood transfusion. This consent verifies that the guardian understands the risks, benefits, and necessity of the procedure. Obtaining this authorization protects both the patient and medical staff while respecting the guardian's rights.
Emergency Blood Transfusion Consent
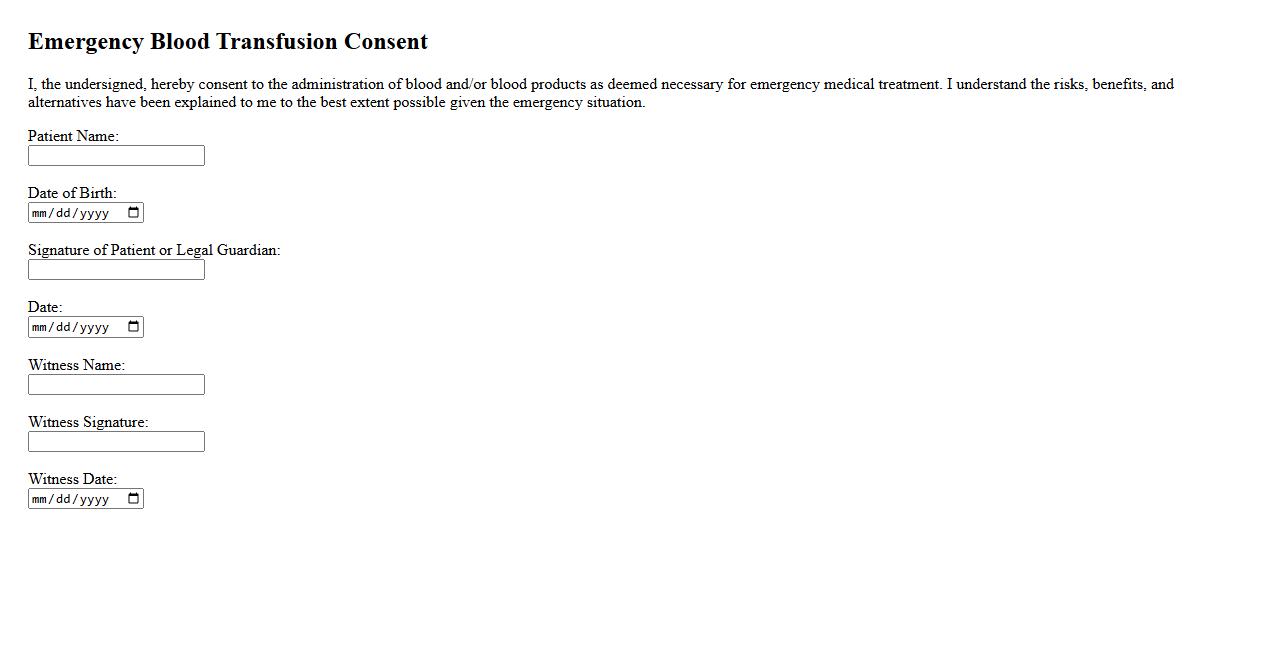
The Emergency Blood Transfusion Consent is a critical authorization given by a patient or their legal representative to allow immediate blood transfusion during urgent medical situations. This consent ensures healthcare providers can act swiftly to save lives without delay for extensive approvals. It is essential for bridging necessary treatment and patient rights in emergencies.
Refusal of Blood Transfusion Agreement
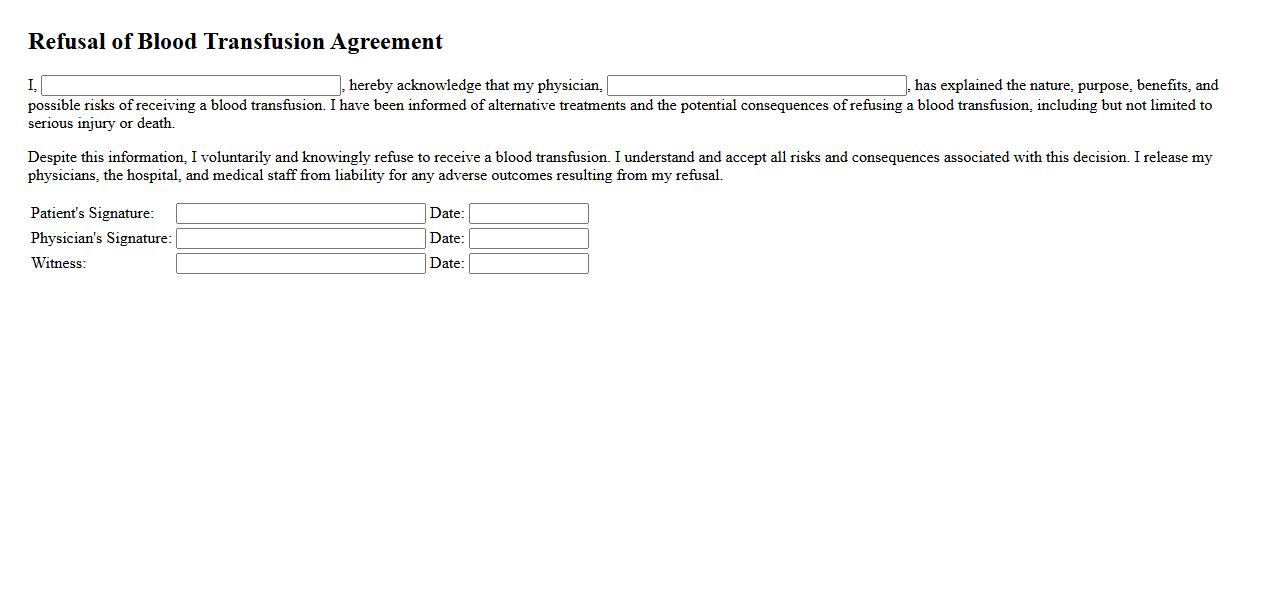
The Refusal of Blood Transfusion Agreement is a legally binding document that allows individuals to decline blood transfusions based on personal, religious, or medical reasons. It ensures that healthcare providers respect the patient's wishes and make informed decisions accordingly. This agreement is crucial for maintaining patient autonomy and preventing unwanted medical procedures.
Blood Transfusion Consent for Minors
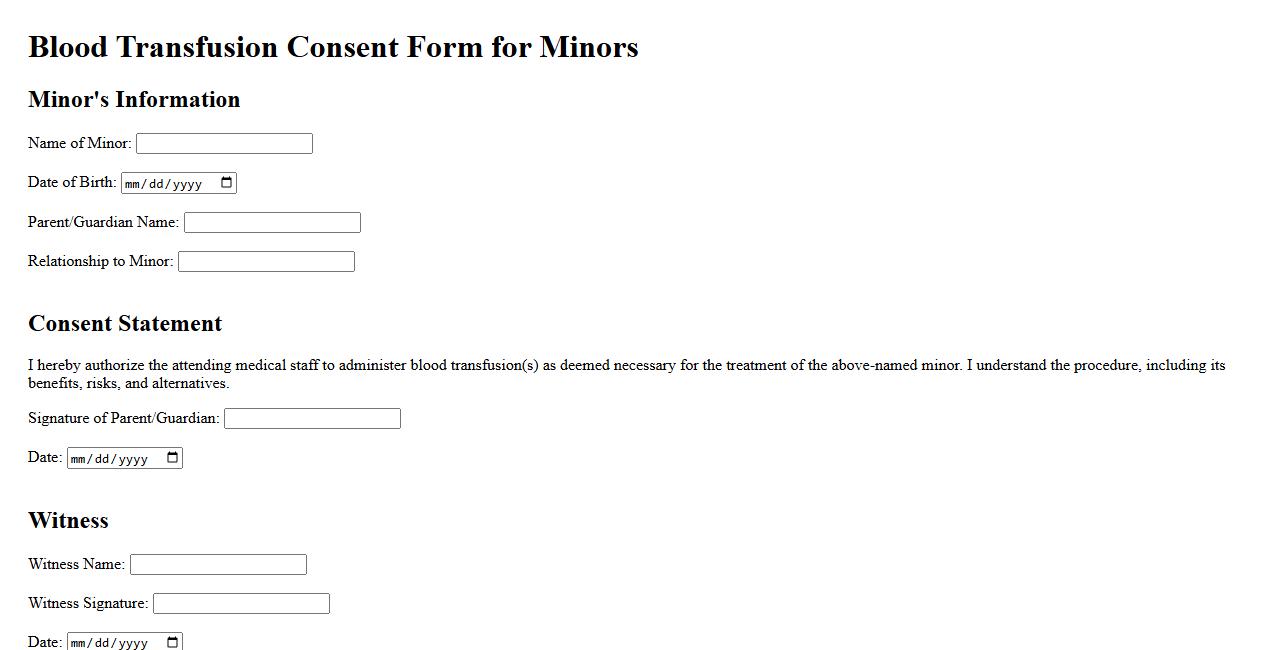
Blood Transfusion Consent for Minors is a critical legal requirement ensuring that guardians or parents authorize medical professionals to administer blood transfusions to patients under the age of 18. This consent safeguards both the minor's health and legal rights during emergency or planned medical treatments. Obtaining proper consent helps maintain ethical standards and protects all parties involved.
Surgical Blood Transfusion Authorization
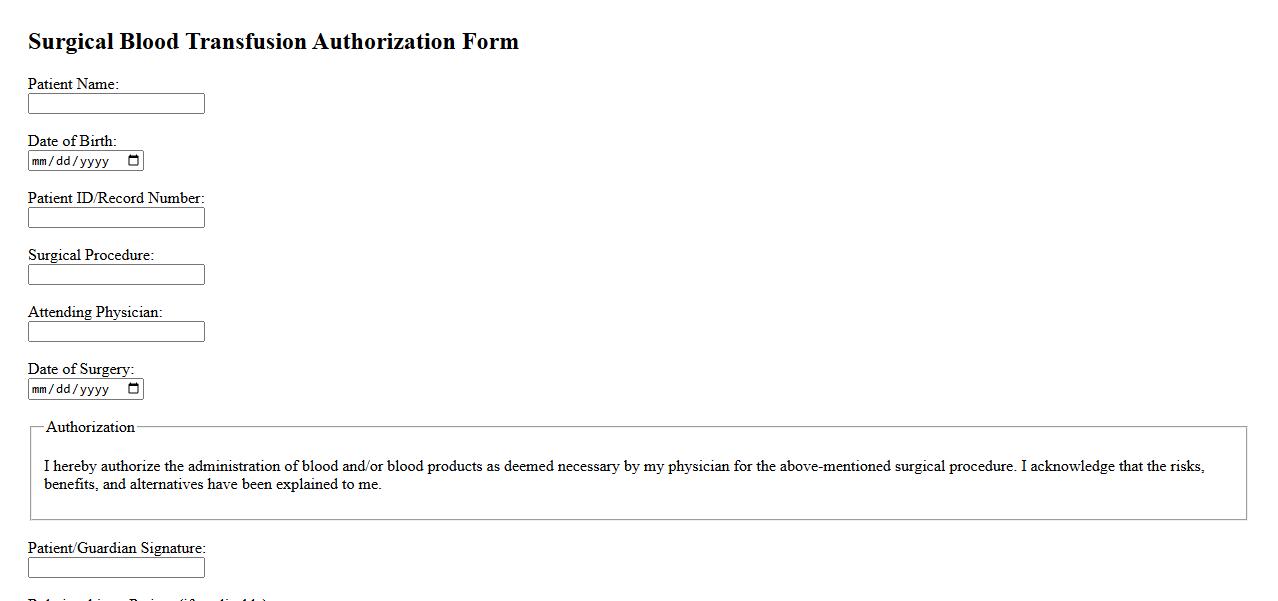
Surgical Blood Transfusion Authorization is a critical document that grants permission for the administration of blood or blood products during surgical procedures. It ensures informed consent has been obtained from the patient or their legal representative. This authorization helps maintain patient safety and compliance with medical regulations.
Transfusion of Blood Products Consent
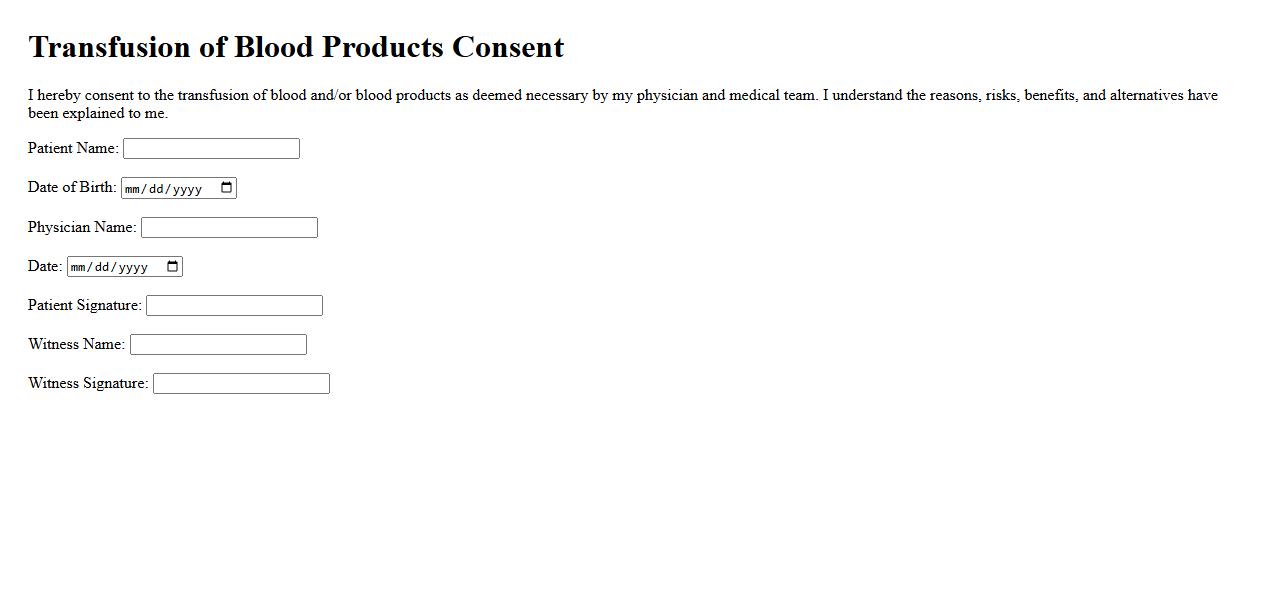
The Transfusion of Blood Products Consent is a vital document that ensures patients are fully informed about the benefits and risks associated with receiving blood transfusions. It serves as a legal agreement between the patient and healthcare provider, confirming voluntary consent prior to the procedure. This consent helps safeguard patient rights and promotes clear communication during medical care.
Multilingual Blood Transfusion Consent
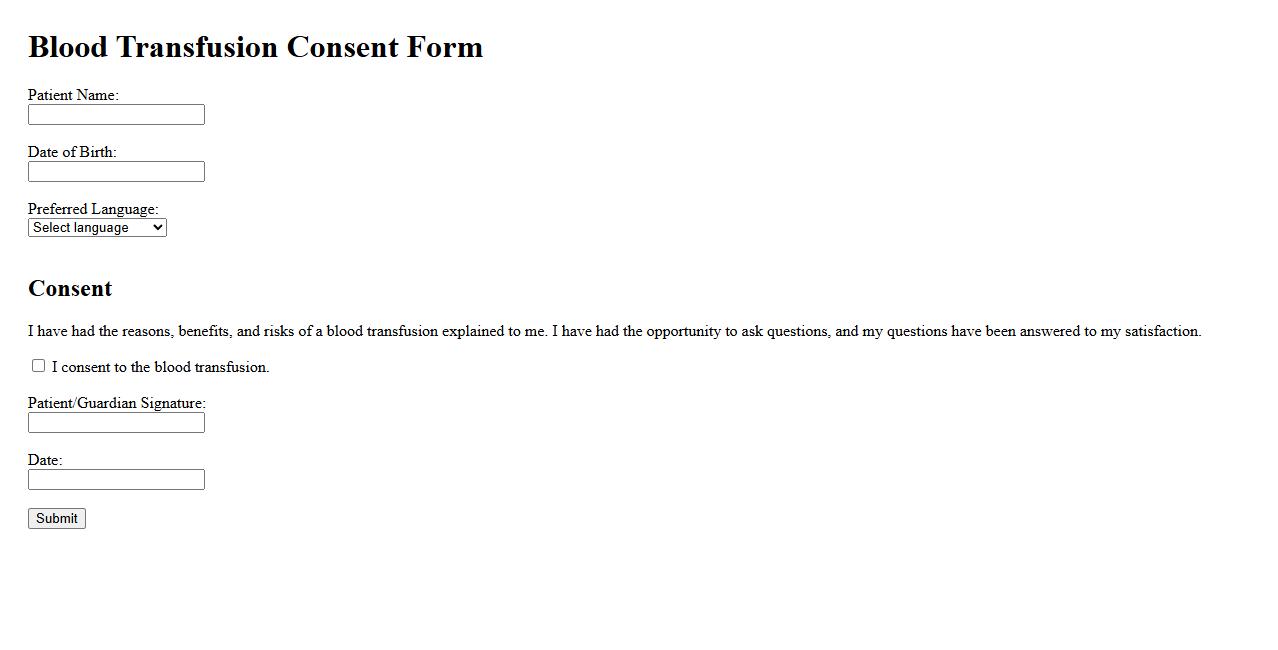
The Multilingual Blood Transfusion Consent form ensures clear communication between healthcare providers and patients who speak different languages. It facilitates informed consent by providing essential information about the blood transfusion process in multiple languages. This approach enhances patient understanding and safety during medical procedures.
Preoperative Blood Transfusion Consent
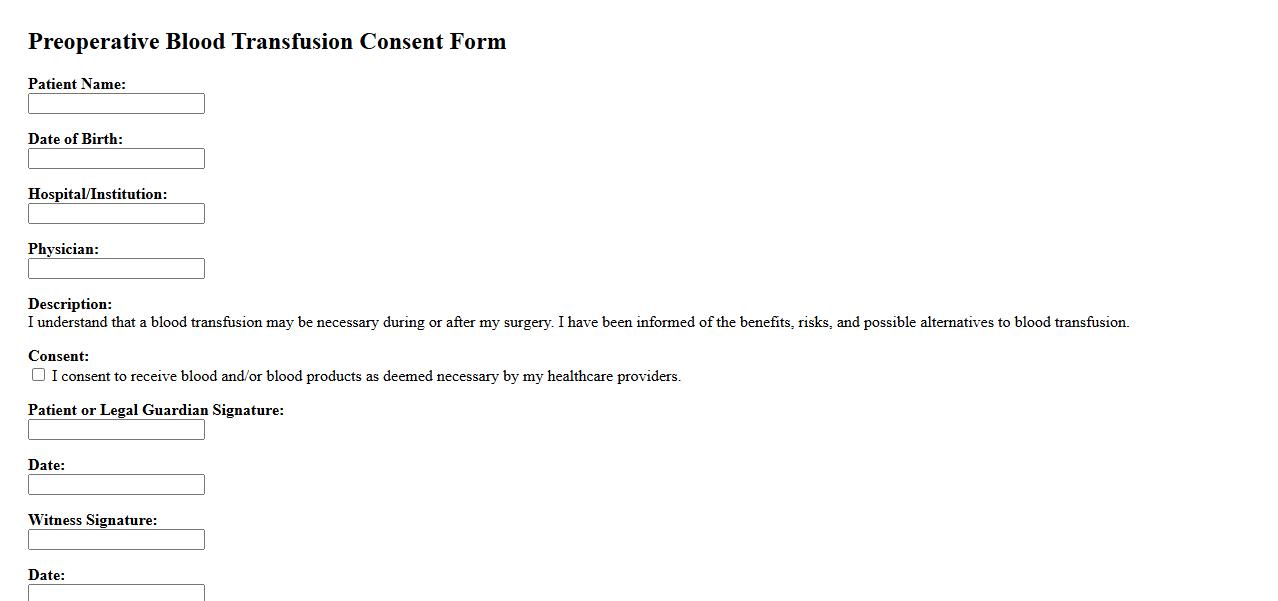
The Preoperative Blood Transfusion Consent is a critical document that ensures patients are fully informed about the risks and benefits of receiving blood transfusions before surgery. It safeguards patient rights by documenting their voluntary agreement to the procedure. This consent process enhances communication between healthcare providers and patients, promoting safer surgical outcomes.
Blood Transfusion Consent for High-Risk Patients
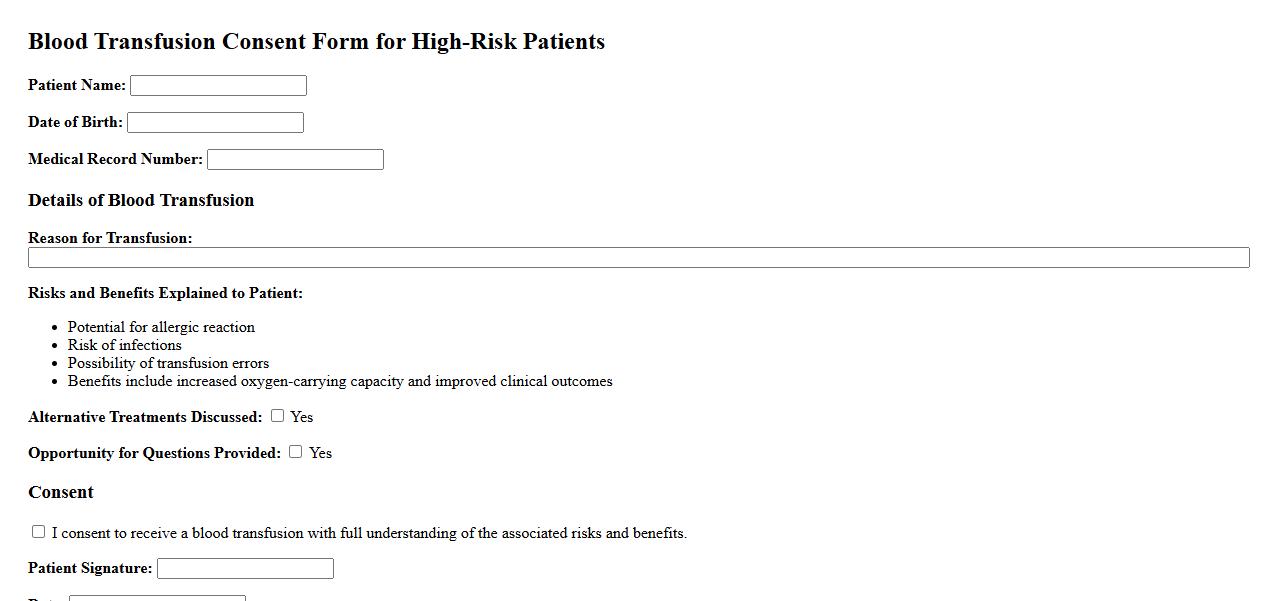
Obtaining blood transfusion consent for high-risk patients is crucial to ensure they understand the potential risks and benefits involved. This process involves clear communication about possible complications, alternatives, and the necessity of the transfusion. Proper documentation safeguards both patient rights and healthcare provider responsibilities.
What is the primary purpose of obtaining consent for a blood transfusion?
The primary purpose of obtaining consent is to ensure that the patient agrees to the procedure after being fully informed. It respects patient autonomy and supports ethical medical practice. Consent also protects healthcare providers legally.
Which key risks and benefits should be explained to the patient before consent?
Patients must be informed about both the risks and benefits of the transfusion. Key risks include allergic reactions, infections, and transfusion reactions. Benefits include improved oxygen delivery and stabilization of blood volume.
What information must a patient understand to provide informed consent for transfusion?
Informed consent requires understanding the nature of the transfusion, potential complications, and alternative treatments. The patient should be aware of the expected outcomes and the reasons for the transfusion. Clear communication ensures the decision is made voluntarily.
Who is authorized to obtain and witness consent for a blood transfusion?
Typically, a qualified healthcare professional such as a physician or nurse is authorized to obtain and witness consent. This individual must be knowledgeable about the procedure to answer patient questions. Documentation of consent is an essential part of the process.
In what situations is it acceptable to proceed without documented consent for transfusion?
Proceeding without documented consent is permissible in emergency situations where there is immediate risk to the patient's life. This is done to prevent serious harm or death when obtaining consent is impossible. Legal and ethical guidelines support this exception.
