
Consent to Treat is a legal and ethical requirement whereby a patient voluntarily agrees to receive medical care after being informed about the risks, benefits, and alternatives. It ensures that healthcare providers respect patients' autonomy and decision-making rights. Obtaining proper Consent to Treat protects both patients and practitioners in medical settings.
Medical Treatment Authorization Form

The Medical Treatment Authorization Form is a crucial document that grants permission for medical care in emergency or non-emergency situations. It ensures that healthcare providers can act swiftly on behalf of patients, especially minors or individuals unable to consent. This form is essential for safeguarding health and facilitating timely medical interventions.
Patient Consent Agreement
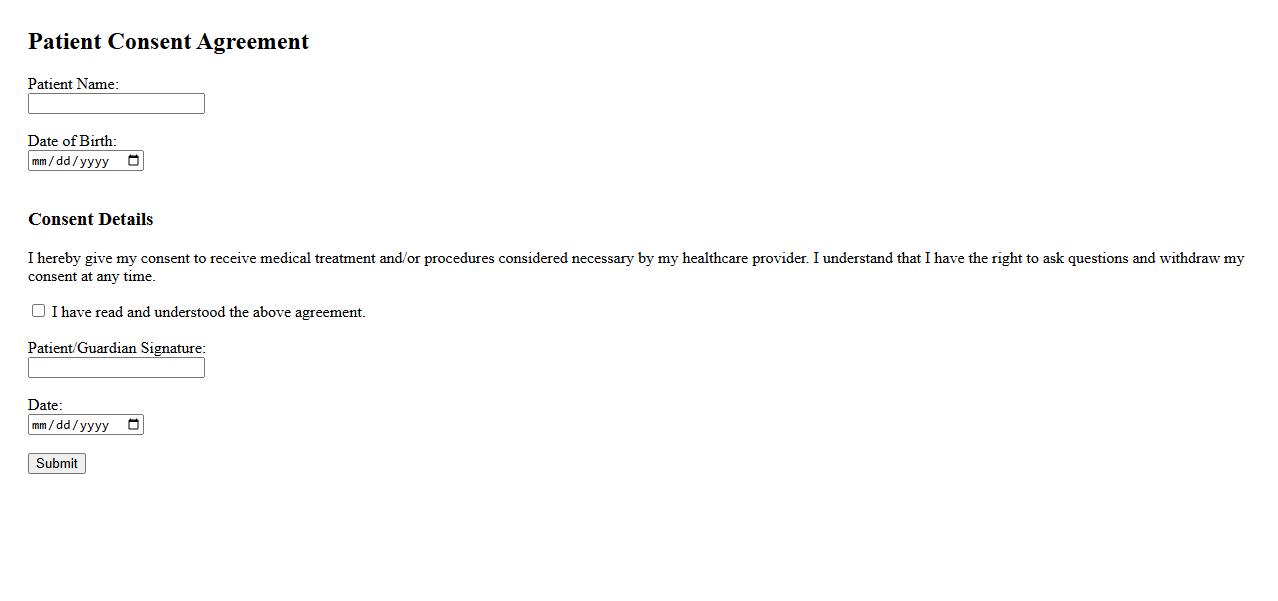
The Patient Consent Agreement outlines the terms and conditions under which medical treatment is provided. It ensures that patients are fully informed about the procedures, risks, and benefits before agreeing to receive care. This agreement protects both the patient's rights and the healthcare provider's responsibilities.
Informed Consent Document

The Informed Consent Document is a critical legal and ethical requirement in healthcare and research, ensuring participants understand the risks and benefits before agreeing to procedures or studies. It provides clear, detailed information to facilitate voluntary and educated decision-making. This document upholds patient autonomy and protects both parties involved.
Healthcare Treatment Permission
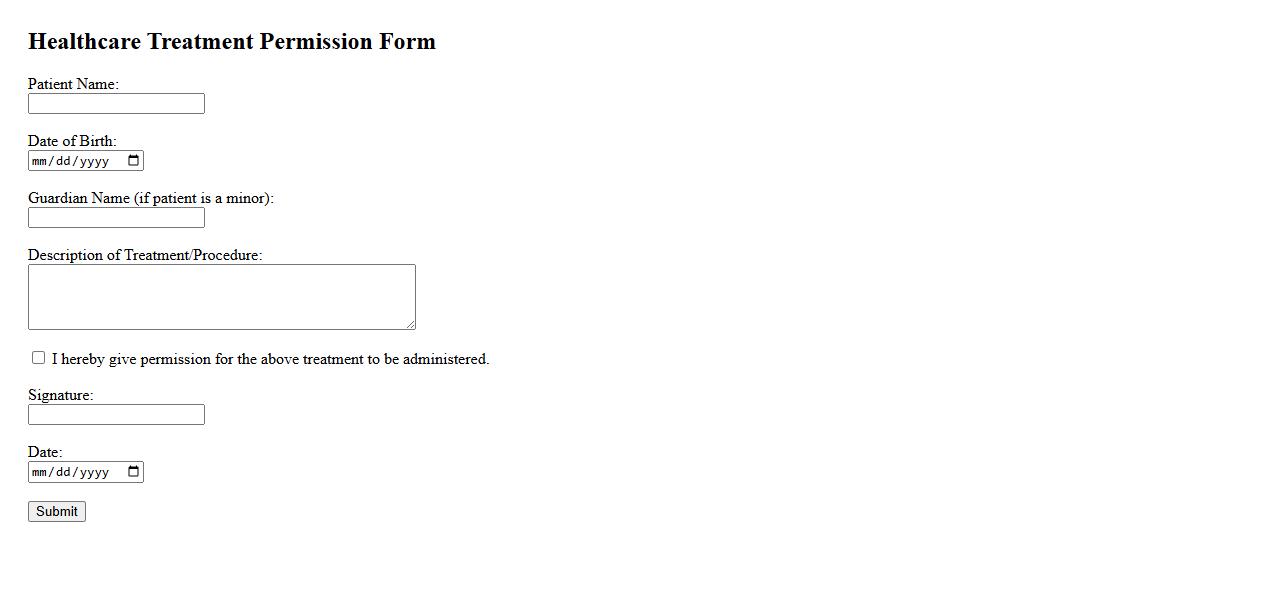
Healthcare Treatment Permission is a crucial consent that allows medical professionals to provide necessary care to a patient. This authorization ensures that treatments and procedures are legally approved, safeguarding the patient's rights and well-being. Obtaining clear permission also facilitates effective communication between healthcare providers and patients or their guardians.
Patient Treatment Approval
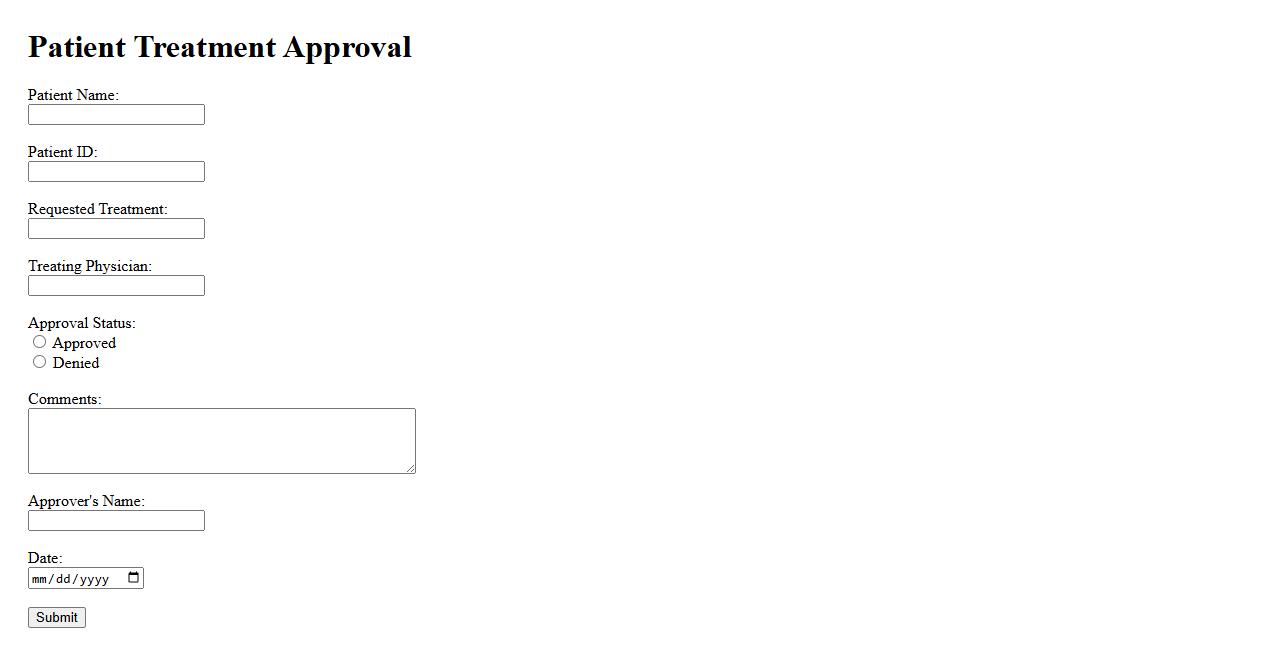
Patient Treatment Approval is a critical process in healthcare where patients or their guardians provide consent for medical procedures after understanding the risks and benefits. This approval ensures that treatments align with the patient's wishes and legal requirements. It fosters trust and communication between medical professionals and patients.
Consent for Medical Procedures
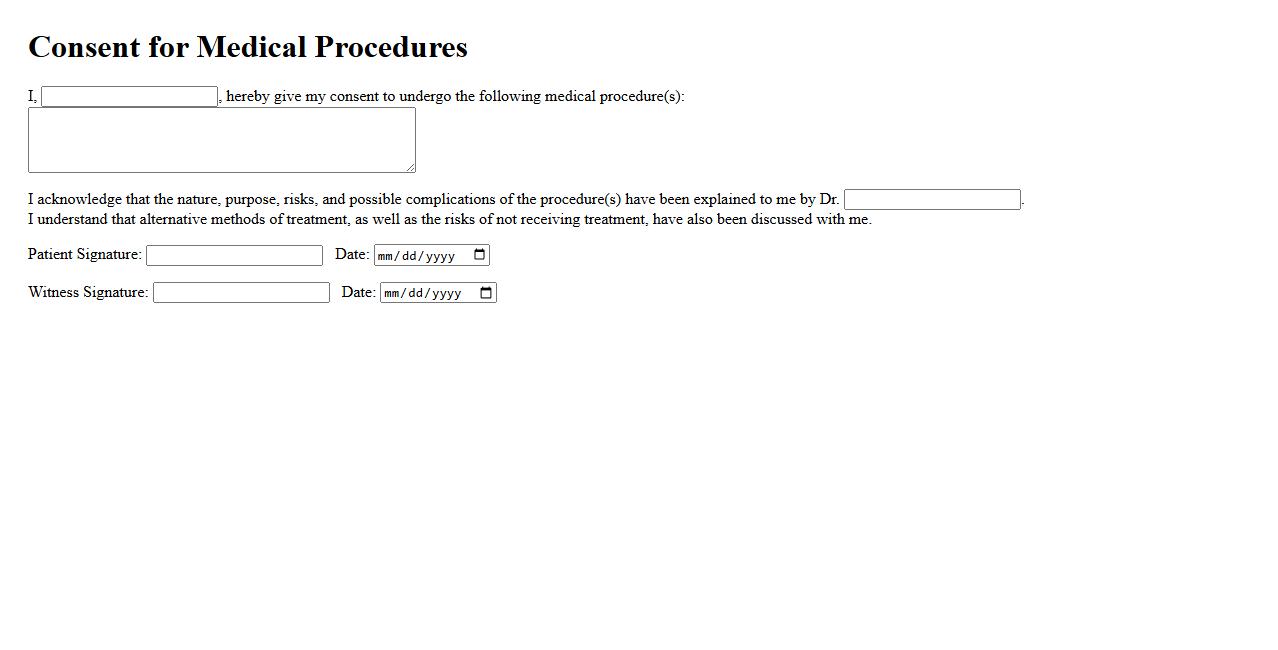
Consent for medical procedures is a crucial process ensuring patients are fully informed about the risks, benefits, and alternatives before undergoing treatment. It empowers individuals to make voluntary decisions regarding their healthcare. Proper consent enhances trust and promotes ethical medical practices.
Authorization for Care

Authorization for Care is a formal approval granting permission for medical treatment or services. It ensures that healthcare providers have consent from patients or guardians before proceeding. This process helps protect patients' rights and facilitates proper healthcare management.
Surgical Consent Form
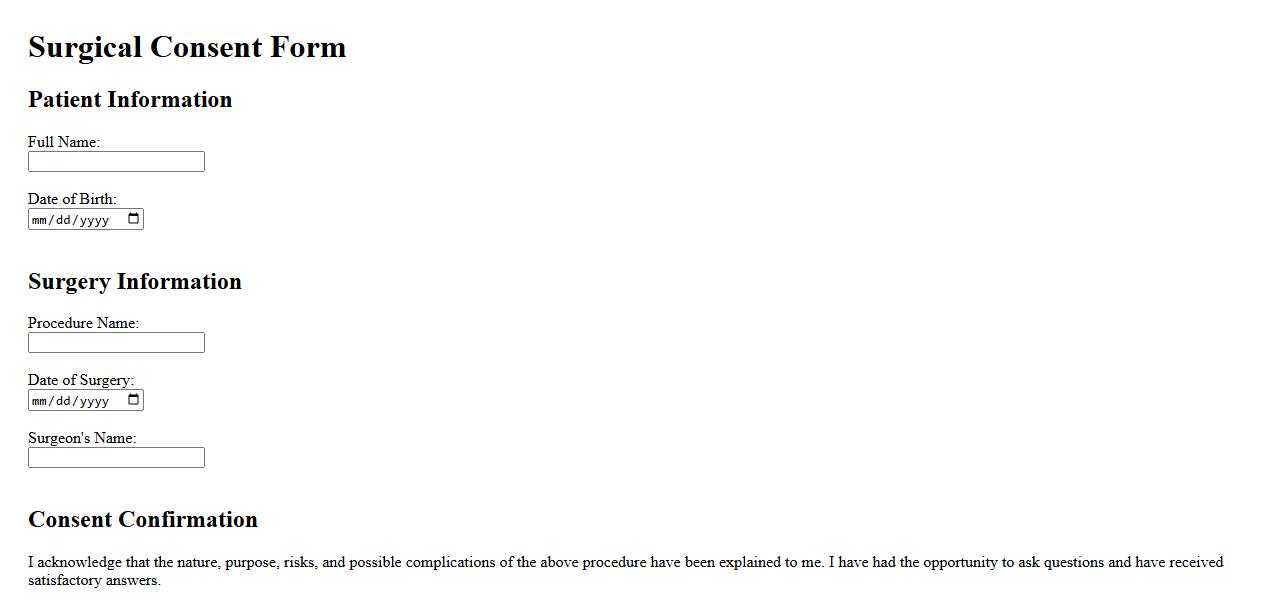
The Surgical Consent Form is a crucial document ensuring that patients understand and agree to the risks and procedures involved in surgery. It provides clear information about the operation, potential complications, and alternative treatments. Signing this form indicates the patient's informed decision to proceed with the surgical intervention.
Treatment Agreement Authorization
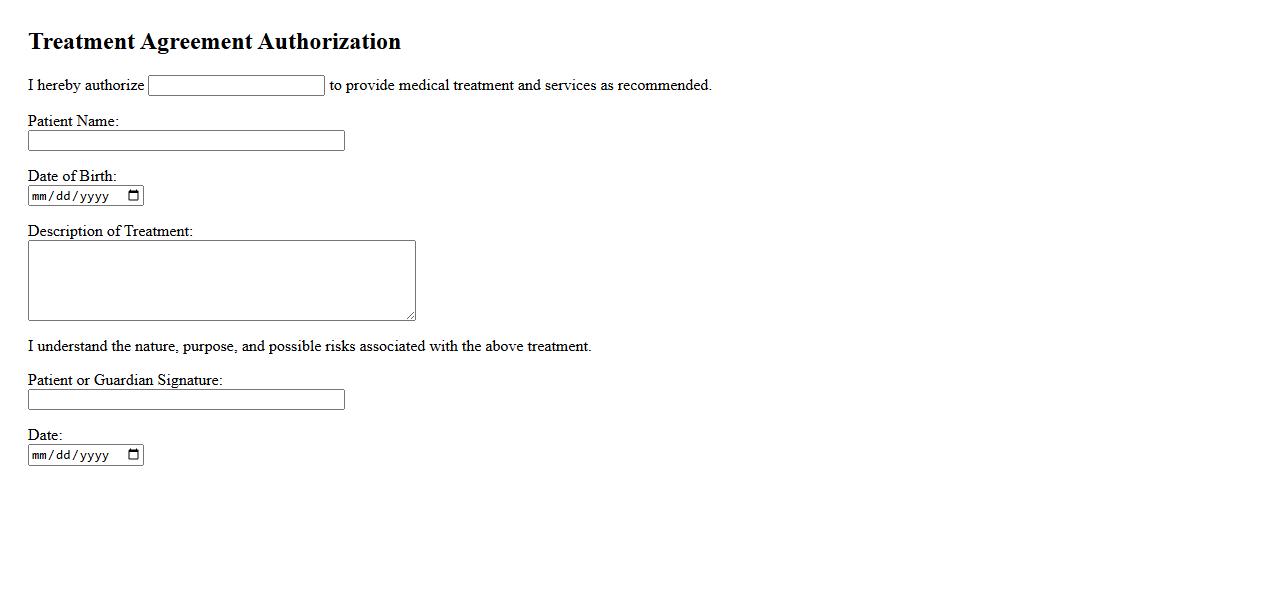
The Treatment Agreement Authorization is a crucial document outlining the terms and conditions between the patient and healthcare provider. It ensures mutual understanding of the treatment plan, responsibilities, and consent to proceed with medical care. This agreement promotes clear communication and protects both parties throughout the treatment process.
Patient Authorization for Services
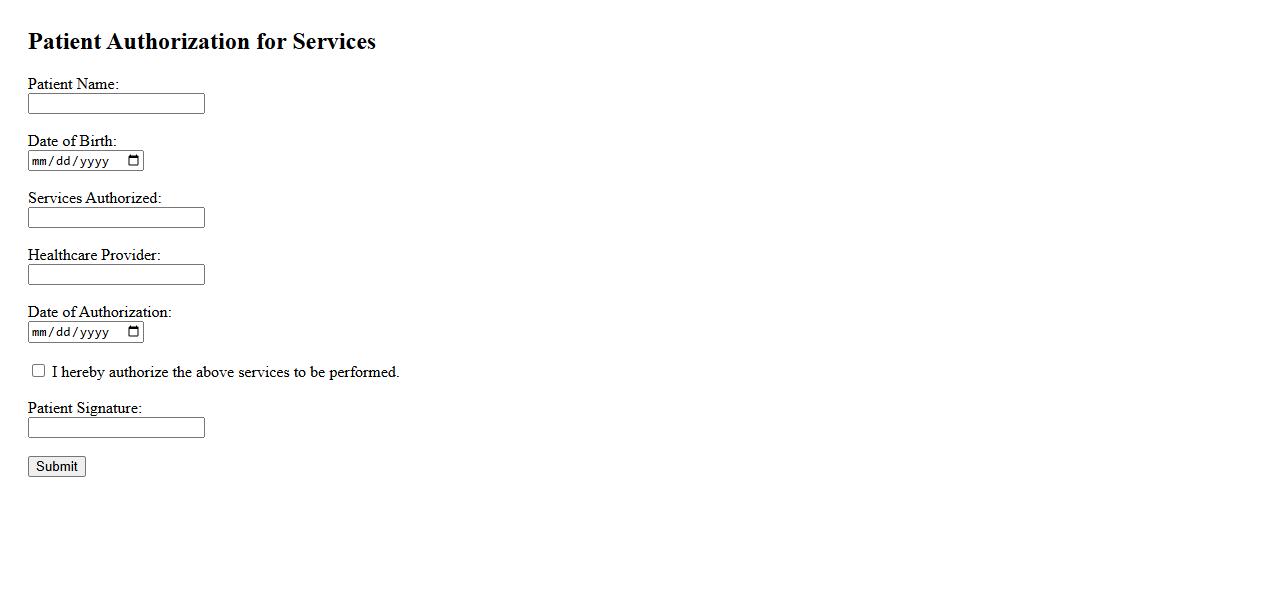
Patient Authorization for Services is a crucial document that grants healthcare providers permission to deliver specified medical treatments. It ensures that patients are informed and consent to the procedures and associated costs. This authorization protects both the patient's rights and the provider's legal obligations.
What key elements must be included in a valid Consent to Treat document?
A valid Consent to Treat document must clearly outline the nature and purpose of the proposed treatment. It should also detail the potential risks and benefits associated with the treatment to ensure the patient is fully informed. Additionally, the consent must be given voluntarily and documented with the patient's signature to be legally effective.
How does informed consent differ from general consent for treatment?
Informed consent involves providing comprehensive information about the treatment, including risks, benefits, and alternatives, enabling the patient to make an educated decision. In contrast, general consent typically covers routine procedures without detailed explanations. Informed consent requires explicit acknowledgement, whereas general consent might be implied through patient registration or treatment initiation.
Who has the legal authority to give consent for treatment in cases involving minors or incapacitated patients?
For minors, legal authority to consent generally rests with a parent or legal guardian, ensuring treatment aligns with the child's best interest. In cases of incapacitated patients, a legally appointed healthcare proxy or power of attorney is authorized to provide consent on their behalf. If no proxy is available, healthcare providers may follow established protocols to proceed in emergencies.
What are the potential consequences of failing to obtain proper consent to treat?
Failing to obtain proper consent can result in serious legal consequences, including allegations of medical malpractice or battery. Healthcare providers risk losing professional licensure and facing civil litigation if patients are treated without valid consent. Additionally, patient trust and institutional reputation can be severely damaged by consent violations.
In what situations can consent to treat be considered implied rather than explicitly documented?
Implied consent typically applies in emergency situations where immediate treatment is necessary, and the patient is unable to provide explicit consent. It is also invoked when a patient voluntarily seeks routine medical care, such as examinations or minor treatments. However, implied consent does not replace the need for explicit consent when possible, especially for invasive procedures.
