
Filing a Claim for Prescription Drug Reimbursement involves submitting proof of purchase and prescription details to your insurance provider or employer for repayment. This process ensures policyholders recover eligible costs associated with prescribed medications. Accurate documentation and timely submission increase the likelihood of successful reimbursement.
Pharmacy Reimbursement Claim Form
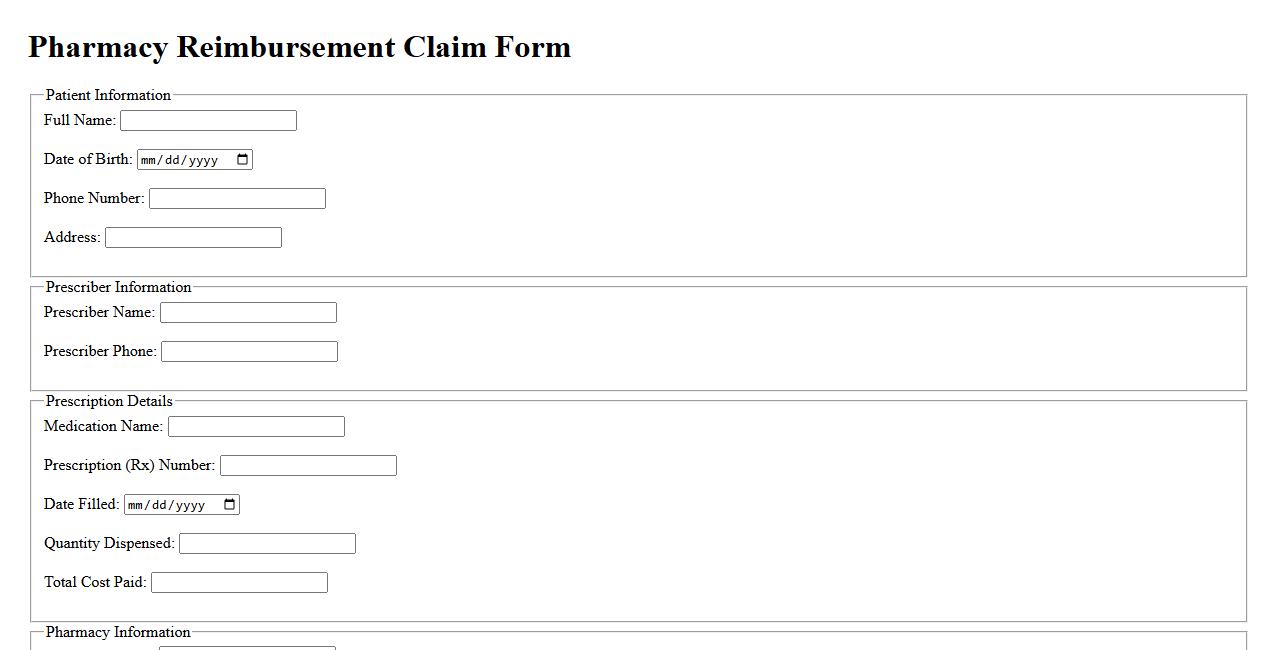
The Pharmacy Reimbursement Claim Form is a crucial document used by pharmacies to request payment for medications dispensed to patients. It ensures accurate processing of claims by insurance providers, streamlining the reimbursement process. Proper completion of this form helps maintain efficient patient care and financial operations.
Medication Expense Reimbursement Request
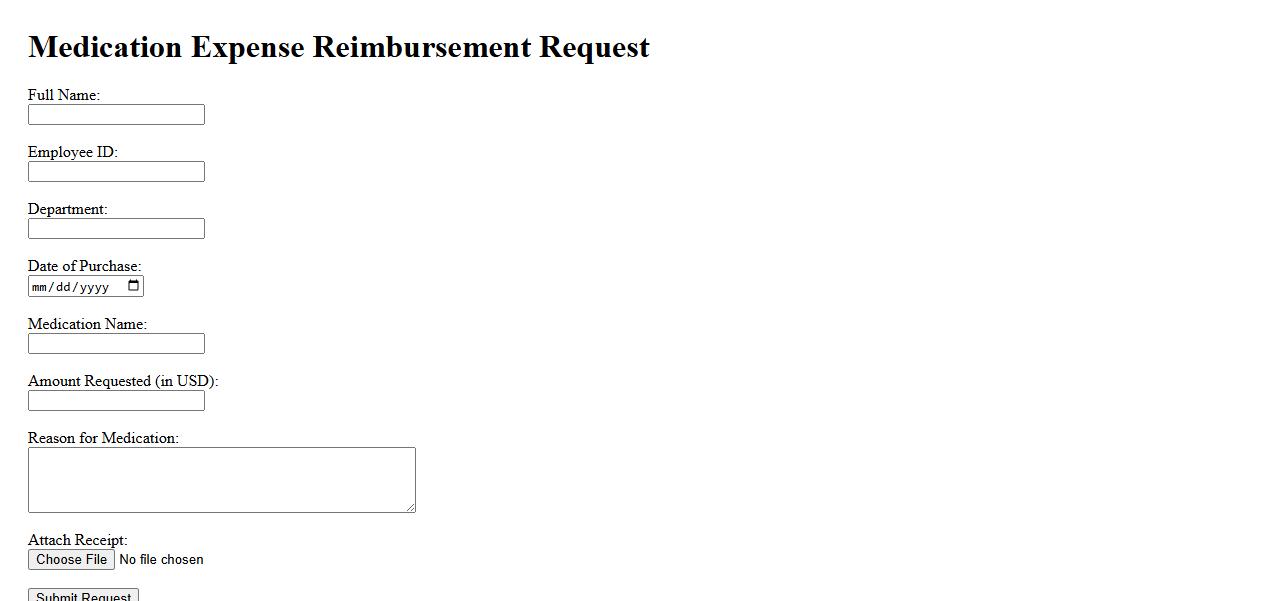
The Medication Expense Reimbursement Request allows individuals to claim back costs incurred on prescribed medications. This process requires submitting receipts and related documentation for approval. Timely submission ensures efficient reimbursement and financial relief.
Prescription Medication Refund Application
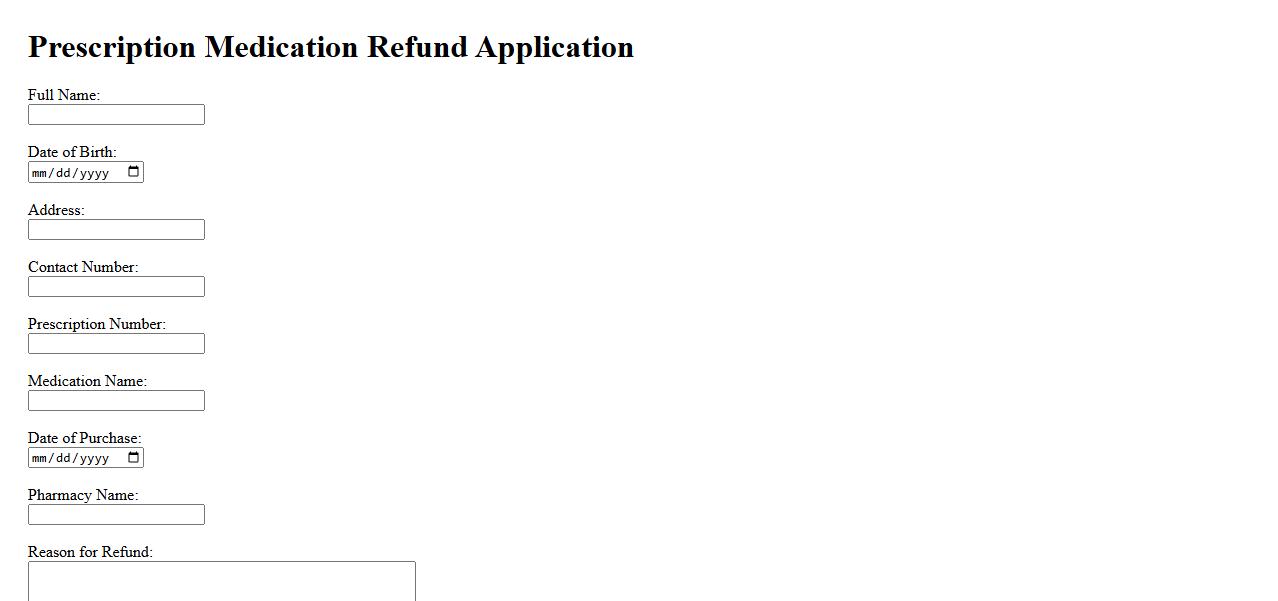
The Prescription Medication Refund Application allows patients to request reimbursement for eligible prescription drug expenses. This process ensures timely refunds by submitting required documentation accurately. Applicants should follow guidelines carefully to maximize their refund approval chances.
Drug Purchase Reimbursement Submission
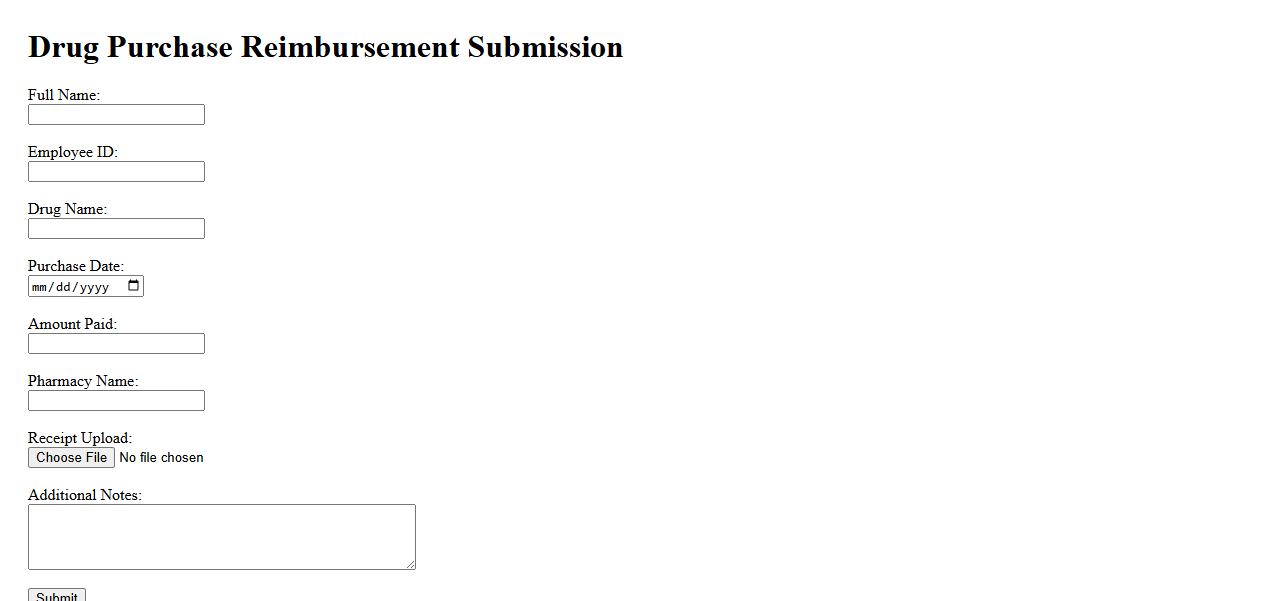
The Drug Purchase Reimbursement Submission process allows patients to claim refunds for eligible medication expenses. It requires the submission of valid receipts and prescription documentation to ensure accurate reimbursement. Timely and complete submissions help streamline the approval and payment stages efficiently.
Out-of-Pocket Medication Claim Form
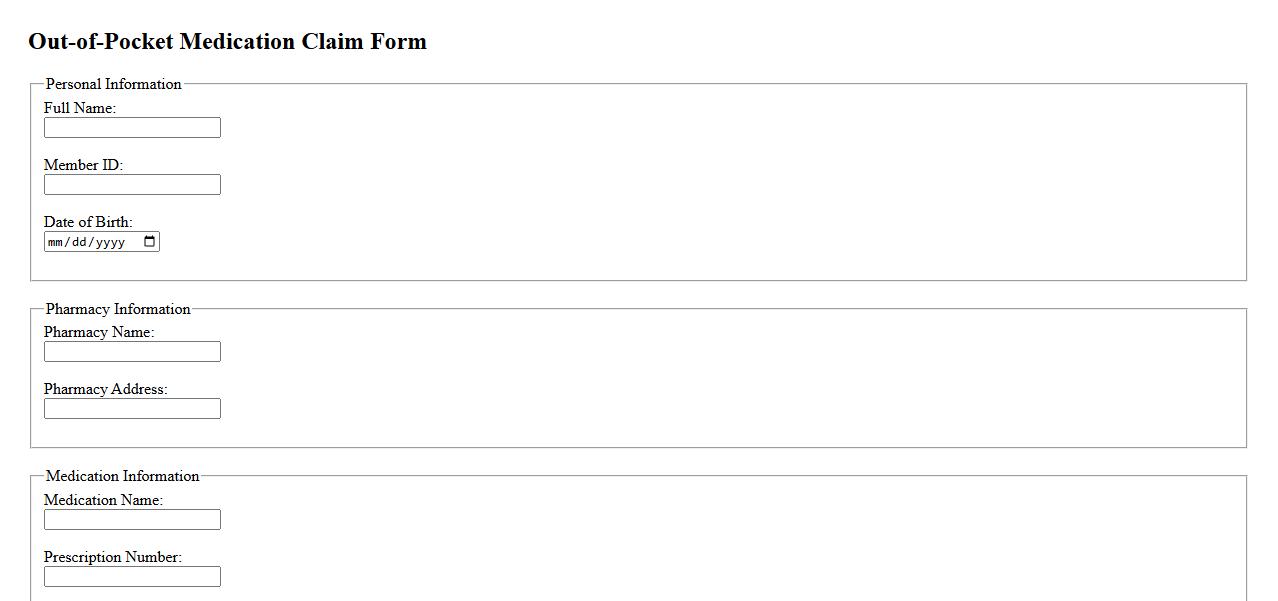
The Out-of-Pocket Medication Claim Form allows patients to request reimbursement for prescription medications paid without insurance coverage. This form ensures accurate processing by documenting essential purchase details and proof of payment. Submitting a completed claim form helps individuals recover eligible expenses efficiently.
Health Benefits Medication Refund Request
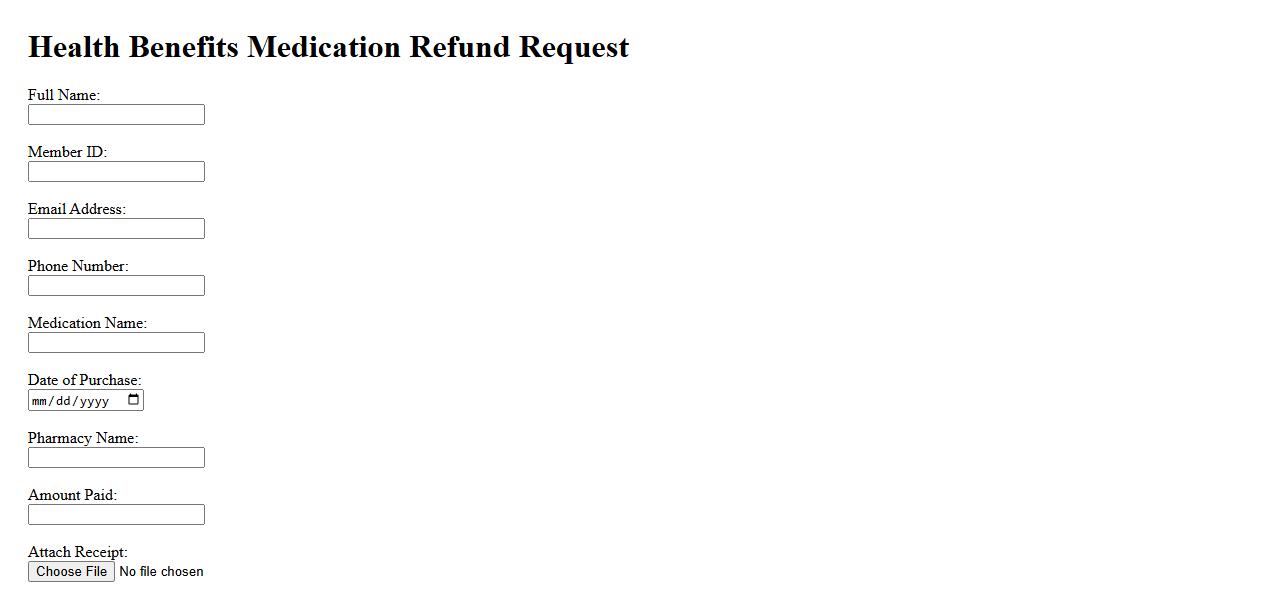
Submitting a Health Benefits Medication Refund Request ensures you reclaim expenses for eligible prescriptions quickly. This process supports managing your healthcare finances efficiently. Timely requests help maintain accurate records and maximize your benefits.
Prescription Drug Coverage Reimbursement Form

The Prescription Drug Coverage Reimbursement Form is essential for claiming refunds on eligible medication expenses. It allows individuals to submit proof of prescription drugs purchased for reimbursement purposes. Proper completion of this form ensures timely processing and accurate reimbursement of prescription costs.
Medication Cost Claim Submission
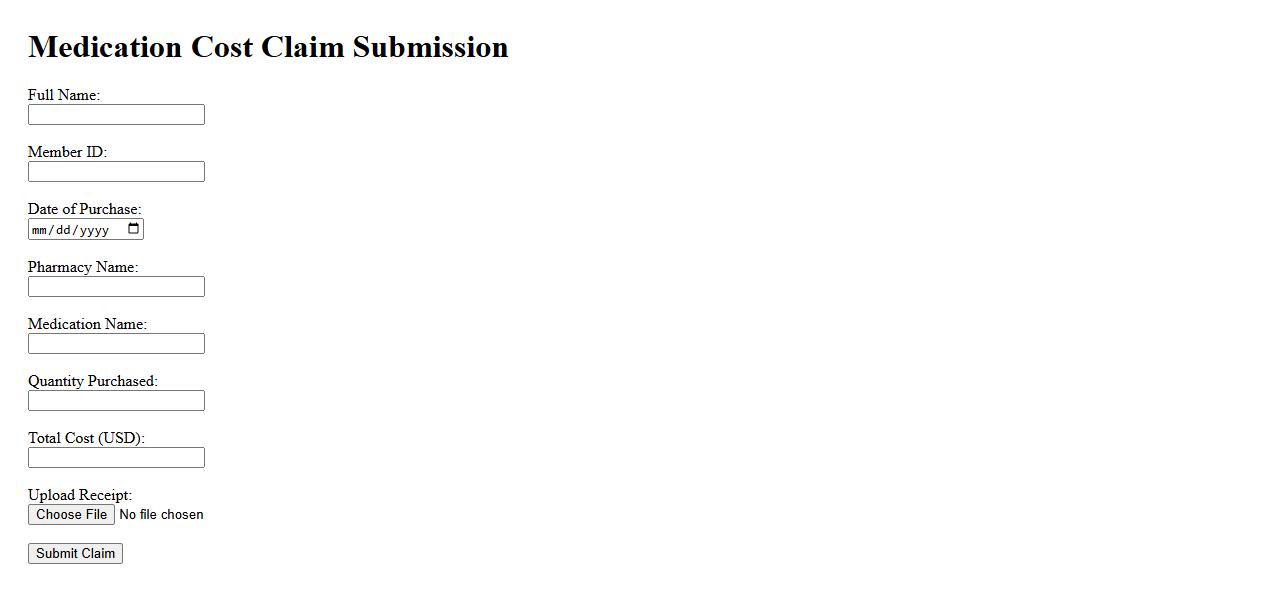
Submitting a medication cost claim involves providing detailed receipts and prescription information to your insurance provider for reimbursement. This process ensures you receive compensation for eligible expenses under your health plan. Timely and accurate claim submission helps expedite the approval and payment of your medication costs.
Prescription Reimbursement Application
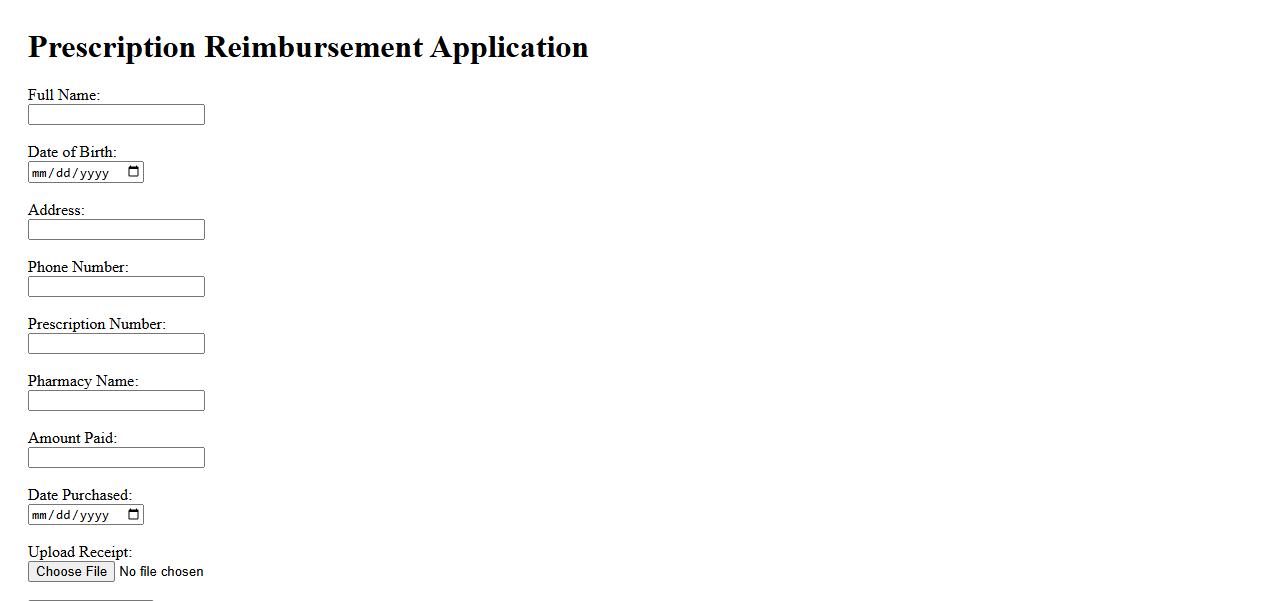
The Prescription Reimbursement Application simplifies the process for patients to claim refunds on eligible medication costs. By submitting necessary prescriptions and receipts, users can efficiently recover expenses from insurance providers. This tool enhances financial accessibility to essential healthcare treatments.
Pharmaceutical Expense Compensation Form
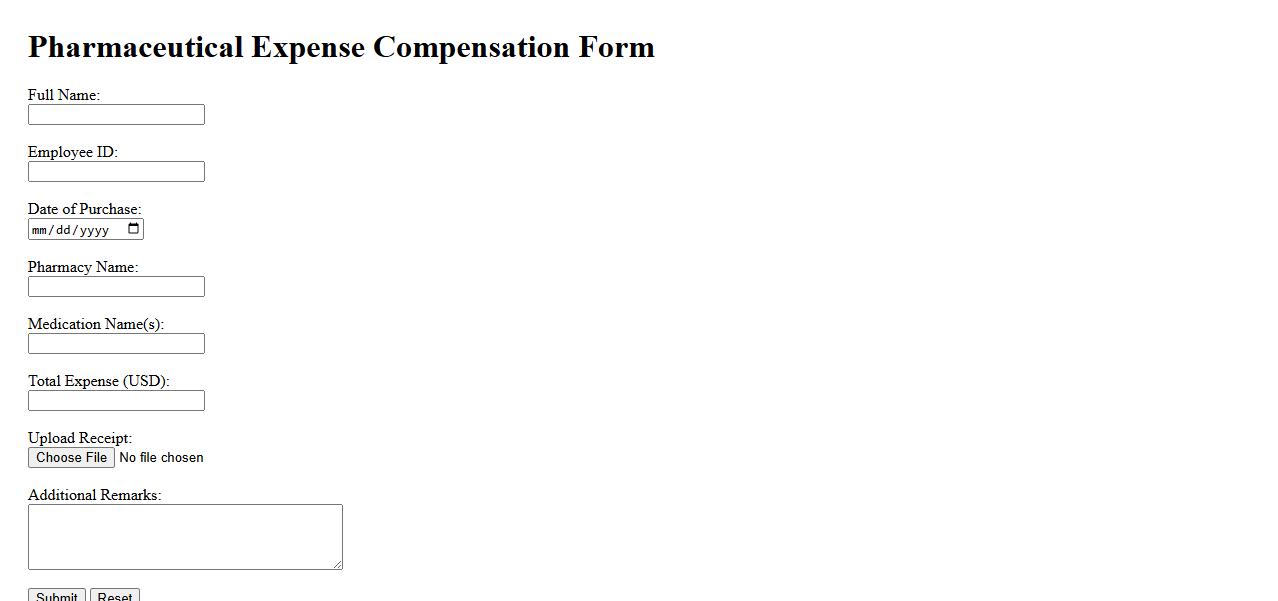
The Pharmaceutical Expense Compensation Form is a document used to request reimbursement for medication-related costs. It ensures patients can recover expenses incurred for prescribed drugs efficiently. This form typically requires detailed information about the pharmaceutical purchase and the claimant.
What information must be included on a claim for prescription drug reimbursement?
A claim for prescription drug reimbursement must include detailed information such as the patient's full name, the prescribing doctor's details, and the pharmacy where the drug was purchased. It should also contain the exact name of the drug, dosage, quantity dispensed, and the date of purchase. Additionally, receipts or proof of payment must be attached to validate the claim.
Who is eligible to submit a prescription drug reimbursement claim?
Eligibility to submit a prescription drug reimbursement claim is generally reserved for policyholders, their dependents, or authorized representatives. The claimant must be covered under the specific insurance or health plan at the time the prescription was filled. Furthermore, prescriptions must be for medically necessary drugs prescribed by a licensed healthcare provider.
Which supporting documents are required for a valid prescription drug claim?
Valid prescription drug claims require original receipts, the detailed prescription from a licensed practitioner, and a completed claim form. Some policies also request a pharmacy invoice specifying the drug name, dosage, and price. These documents must clearly show that the drugs purchased match the terms of the reimbursement policy.
What types of prescription drugs are covered for reimbursement under this policy?
The reimbursement policy generally covers FDA-approved prescription medications that are listed on the insurer's formulary. Coverage often excludes over-the-counter drugs, vitamins, or supplements unless prescribed for a specific medical condition. Additionally, certain high-cost or experimental drugs may require prior approval from the insurer.
What is the process and timeline for submission and approval of a drug reimbursement claim?
The submission process requires filling out a claim form accurately and submitting it along with all supporting documents to the designated insurer address or online portal. Most insurance providers recommend submitting claims within 30 to 60 days from the date of purchase to qualify for reimbursement. Once received, the insurer typically processes and approves claims within 7 to 14 business days, notifying the claimant of the decision.
